In Part 5, we talked about epidemiological implications of overdispersion. In this section, we explore potential CAUSES of COVID-19 overdispersion.
1: VIRAL LOAD
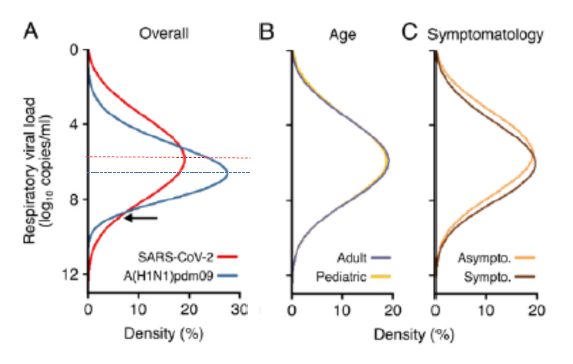
Based on nice system rev by Chen et al, doi.org/10.1101/2020.1, the variability in Respiratory Viral Load for SARS-CoV-2 >> Influenza A across individuals. Interestingly, the mean viral load (VL) is actually lower for SARS-CoV-2 than Influenza, but due to greater individual variability, in SOME cases, the VL is much higher (below arrow).
Furthermore, this greater variability in SARS-CoV-2 VL is not attributable to age or symptomatology.
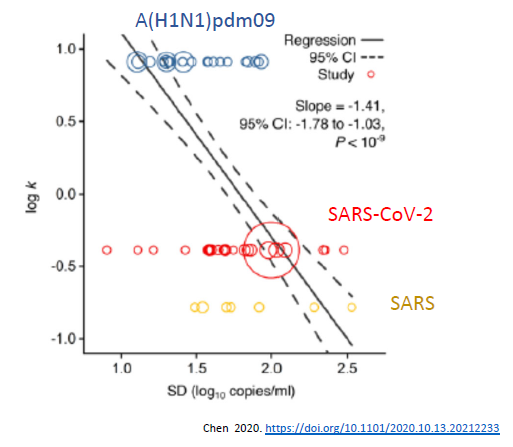
Paul Chen et al makes argument that this greater variability in VL can account for differences in dispersion seen with SARS vs. Influenza. This can be seen in the plot of Dispersion (log k) vs. SD of VL. Greater variability in VL ==> lower k (increased dispersion).
2. DROPLET PRODUCTION
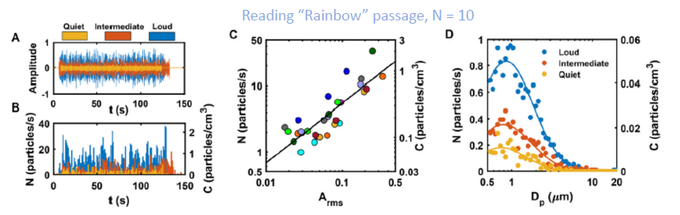
Amount of droplet production can vary markedly by activity, and even by how loud one speaks. This was eloquently revealed by Asadi et al doi.org/10.1038/s41598
Asadi et al asked 10 individuals to read aloud a “Rainbow” passage at 3 different loudness amplitude. As seen below (Middle plot), the louder one spoke, the more droplets were released. The increase in droplet production with greater loudness was seen across droplet sizes (Right) – most notably @ 1 um range (~4x for loud vs. quiet).
It is probably not coincidental that many superspreading events (SSE) occurred during choir practice (e.g. Skagit), religious sites (praying/chanting/singing), in bars (need to talk loud over the din), and meatpacking plants (speak over high levels of noise).
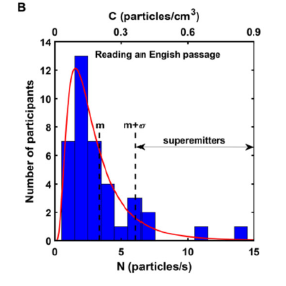
Variability occurs across individuals too. Asadi asked participants (N=40) to read “Rainbow” & “Little Prince” passage at same voice amplitude 85 dB. As seen below, some were “superemitters” – producing much more droplets than others.
NOTE: this variability is not unique to SARS-CoV-2, but ability to do this while infectious (i.e., presymptomatic/asymptomatic) may very well be! I also suspect that SARS-CoV-2 can enhance droplet production for specific physiological reasons (for future thread).
3. VENTILATION
This needs not much intro, because airborne transmission nature of SARS-CoV-2 is widely discussed across Twitter. Many SSE’s have occurred in poorly ventilated venues. However, how does AIRBORNE transmission mode for COVID affect Dispersion?
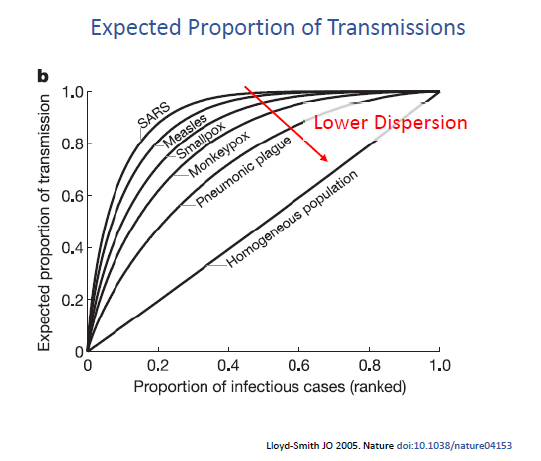
I don’t have the answer, but it’s curious that in Lloyd-Smith’s 2005 landmark paper (nature.com/articles/natur), the pathogen w/greatest dispersion (low k) are “Airborne” (SARS, Measles +SARS2), while ones w/lower dispersion are “Droplet” (Smallpox, Pneumonic +Influenza).
Aerosolization (specifically airborne) predisposes to wider exposure network – so IMO it would make sense that airborne pathogens like SARS-CoV-2 would show patterns of overdispersion. But appreciate hearing from others whether there is data on this.
4. SOCIAL NETWORK, CONTACTS
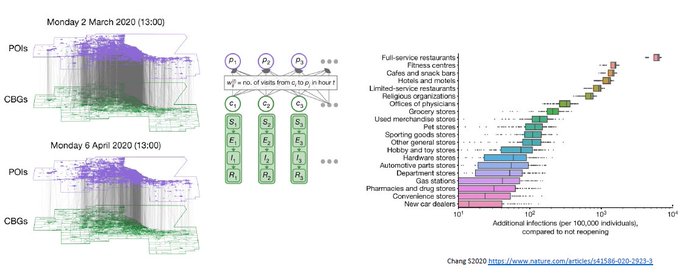
No surprise here, variability in our contacts (social networks) account for variations in COVID-transmission. This includes not only WHO you interact with, but also WHERE, as shown by Chang et al (nature.com/articles/s4158). e.g., Restaurants.
NOTE: again, this social contact variability is not unique to SARS-CoV-2, but ability to socialize while infected (i.e., presymptomatic/asymptomatic) may be one of its distinctive features.
5. SUSCEPTIBILITY
Probably the least appreciated factor when it comes to overdispersion. Lost in the fact that at SSE’s – like choir practice or bars – not only are index cases singings/talking loud, but so are the infectees! Larger tidal volumes increase chance of infection.
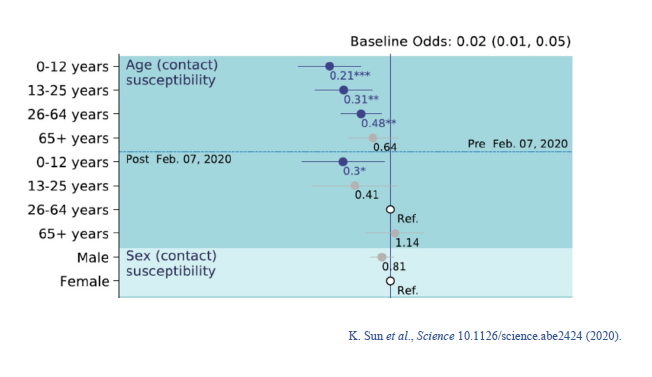
Variability in susceptibility exists not only w/activity, but also by individual. E.g., older individuals are more likely to be infected, less so for younger (Fig: from Sun et al science.sciencemag.org/content/early/ – Suppl). (This may be different for variant B.1.1.7)
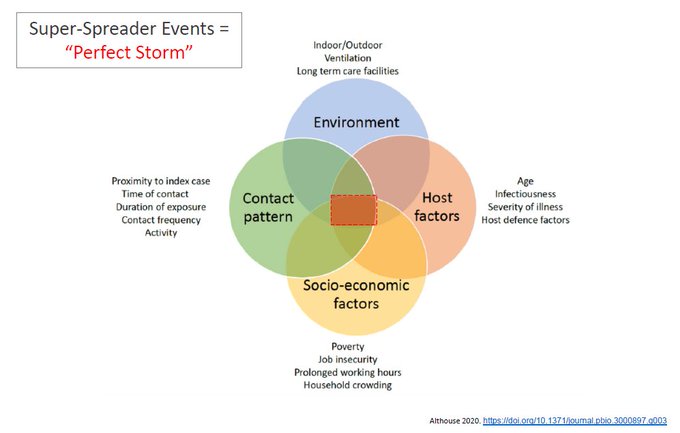
Ultimately, combination of these factors (each accounting for variable transmissions) likely lead to the overdispersion of COVID-19. Importantly, SSE’s occur when all factors align to create a “Perfect Storm” where transmission is maximized. (fig: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7543342/ )
This is my sincere attempt at explaining why COVID-19 may be overdispersed; but def not final word. Welcome any thoughts.